Due to COVID-19 restrictions ASCO’s annual meeting will take place virtually this year… and we’re going to be taking part!
ASCO will be delivering the latest cancer science to the global community via a Virtual Scientific Program. The program will feature over 250 oral abstract presentations and 2,500 poster presentations in 24 disease-based and specialty tracks.
Jeremy Smith, Mary Dominiecki, Alex Kalmanofsky, Dori Stern, Meredith Jacobetz and Genevieve White will be attending from The Planning Shop.
If you’re attending the meeting and you’d love to chat about any of the presentations or findings, please get in touch with us or look for our team online at the event. We’d love to hear from you.
By Yvette (Wei-Yu) Ke
When it comes to healthcare there are different opinions about patient care East and West, and as market researchers, understanding this is critical. Yvette (Wei-Yu) Ke from The Planning Shop explains why.

In Changchun, China, a family discovers their Nai Nai (grandmother) has been diagnosed with terminal cancer and seemingly only has a short time to live. Their discussions are instinctive: ‘’If you tell her, will you ruin her good mood?’’. Their conclusions: “Yes”.
The family decide to keep the diagnosis from Nai Nai and instead hastily arrange a wedding for a grandson who has only been in a relationship for a few months. The wedding is pitched as a chance for a family reunion, but in reality, it’s an excuse for a final farewell. Nai Nai is excited, and completely unaware that the benign shadows on her scans are anything but and foretell a fatal end.
Does this sound like a Hollywood drama? It should because it’s the plot for a much-talked-about new Hollywood movie called ‘The Farewell’. However, it’s not just a film as this happens all the time in parts of East Asia, including Japan and Singapore.
For many in the Western world it may come as a surprise that a family could do such a thing, but having grown up in Taiwan, this scenario is neither surprising nor unusual. If I were to knock on my neighbours’ doors back home, it would be easy for me to find a family going through a similar scenario. In fact, it even happened to my family…
Back in 2013, when my grandmother was diagnosed with colorectal cancer at the age of 89, a family meeting was called to discuss what to do next. If we told our grandmother the truth, she would no longer enjoy her twilight years: meeting friends, playing with her grandchildren and celebrating important festivals and events. She’d also become sensitive to how she looked, what she ate or how much she slept. As a family, we knew we had a responsibility to keep her away from these worries, and a duty to carry the burden for her.

As we are very ‘Xiao-Shun’, we decided not to tell her. We agreed to arrange the surgery to remove the malignant tumour in her body, without telling her what the surgery was for.
‘Xiao-Shun’ translates as filial piety – or more simply put respecting your elders and looking after them. Traditionally, there is a lot of pressure and criticism from society if you don’t demonstrate ‘Xiao-Shun’.
Two weeks before the surgery, we took our grandmother to hospital to discuss pre and post care. The surgeon, anaesthetist, radiologist, nutritionist and case manager were all there. When we saw them, the first thing we did was hand over a slip of paper that said, “Our grandmother doesn’t know she has cancer”, just in case any of them leaked our secret. The surgery went ahead.
My grandmother will turn 95 this year and she is particularly proud that amongst her siblings she is the only one who has never had cancer! To this day she still doesn’t know the truth. Maybe this belief is one of the reasons she’s alive and well.
Why am I telling you this story and talking about ‘The Farewell’? Because, as a global healthcare market researcher, I believe it’s important to understand different cultures, and what drives patient care across a variety of societies, nations, traditions and backgrounds. How can we ever understand the needs and drivers for different treatments and pharmaceutical products unless we truly understand the decision-making processes and who makes those decisions?

What are the other differences?
As a Taiwanese living and working in London, I’ve experienced how Western culture puts greater emphasis on the individual, their personal freedom and right to privacy, and how this is different from the Eastern way of collectivism, family focus and harmony.
With family playing a central role in Eastern culture, family-based decision-making happens for all parts of life, not just healthcare and treatment choice. In my grandmother’s case, our family was heavily involved in the decision-making process. From which doctor she needed to see, the need for and type of surgery (minimally invasive or traditional with an implant) and post-surgical care. Despite the fact my grandmother was competent enough to make her own choices, she happily followed our decisions. Especially as there is satisfaction and honour to be had in being protected by the children she spent her entire life taking care of.
Studies suggest 30-50% of cancer patients in China have a diagnosed condition concealed from them and over half of family members consider withholding a cancer diagnosis from the patient. (Footnotes 1-3)
Aside from cultural taboos, insufficient legal framework and a lack of awareness of patient rights, this statistic is fuelled by other socio-demographic factors. Families are often afraid to cope with a patient’s emotional reaction or they may simply be unable to afford recommended treatments.
In China, physicians tend to go along with nondisclosure requests from families to avoid patient conflict and even violence. Several cases exist where doctors have informed patients of their diagnosis, without the family’s permission, and have then been reported or faced legal action.
Violence towards medical staff is also an issue, on average 27 such attacks are reported in each hospital in China every year (with countless others not reported or settled with pay-offs). Violence in China’s healthcare system is another story in itself, but you can begin to understand why physicians are often willing to cooperate in non-disclosure agreements with family members. (Footnote 4)
In Western society it seems inconceivable that patients would not be told this type of information. Occasionally we hear of requests from family members to withhold information from patients – particularly when they become substitute decisionmakers closely involved in patient care. However, patient autonomy is entrenched in Western healthcare systems. This notion triggers several ethical issues and not to mention the legal and civil implications.
This contradiction poses an interesting challenge in truly understanding patient experiences and how we leverage these for global brands and patient support initiatives.
Change is coming
Over the next few decades I expect things in Asia to change. With an increased level of awareness about patient rights in younger generations and new legislation emerging, this culture of non-disclosure will certainly evolve. In January 2019, Taiwan passed the ‘Patient Right to Autonomy Act’, the first country in Asia to introduce this type of law. Many hospitals in Japan also self-regulate that patients should be informed of their diagnosis unless they have agreed otherwise.
There’s also a lot the West can learn from the Asian model. In fact, we’re beginning to see Western systems increasingly adopt the concept of patient and family-centred care. This does not mean patients are deprived of making their own healthcare decisions, but the aim is to promote the importance of family members’ roles in the patient’s healthcare experience, improving patient outcomes and support plus greater satisfaction for healthcare professionals.
One size never fits all
Patient experiences are complicated, subject to constant change and highly dependent on healthcare systems, the services available, culture and society. In healthcare market research we often see US and European-based companies applying a Western centric perspective to the rest of the world. This lack of understanding of some aspects of Eastern culture could lead to research outcomes that do not fit with local practices, which in turn creates gaps when trying to draw one global patient experience.
Eastern countries are now promoting patient-centric care to balance the heavily involved family element, and the West is starting to integrate family decision making and support. It’s interesting because this means differences in patient experiences should become less pronounced over time with a convergence of Eastern and Western values.
For now, though, we must never forget the considerable importance of understanding the impact of differing cultures, customs and traditions when devising and interpreting healthcare market research solutions.
P.S. If you ever meet my grandmother, please don’t tell!
References:
1. ‘Disclosure of cancer diagnosis in China: the incidence, patients’ situation, and different preferences between patients and their family members and related influence factors.’ Yuxiu Liu, Jinhong Yang, Da Huo, Honghua Fan, Yufang Gao. 2018 10: 2173–2181.
2. ‘Is therapeutic non-disclosure still possible? A study on the awareness of cancer diagnosis in China.’ Wang DC, Guo CB, Peng X, Su YJ, Chen F. Support Care Cancer. 2011;19(8):1191–1195.
3. ‘Quality of life in Chinese home-based advanced cancer patients: does awareness of cancer diagnosis matter?’ Fan X, Huang H, Luo Q, Zhou J, Tan G, Yong N. J Palliat Med. 2011;14(10):1104–1108.
4. ‘Under the Knife: Why Chinese patients are turning against their doctors.’ Christopher Beam, The New Yorker, August 18, 2014
About the author

Yvette (Wei-Yu) Ke is a Research Manager within the Quantitative Centre of Excellence at The Planning Shop She began her pharmaceutical consultancy and market research career in Taiwan where she built up her strong knowledge in Asian markets. Since then she has extended her career in the UK to develop her experiences across global markets.
Download a pdf version of the article here.
During a pandemic, it’s important to continue with healthcare market research to keep sight of the advances the industry needs to make in the prevention and treatment of many other diseases. We still need advances in cancer, cardiology, and rare diseases. We still need to listen to patients who are not only suffering from COVID-19, but who are suffering from diabetes, hemophilia and neurological conditions. We still need to engage with oncologists, hematologists and ophthalmologists. But we need to be mindful how we do this. We need to show relevance when asking people for their time. And we need to show understanding for the unusual situation many doctors and patients are currently finding themselves in because of the pandemic.
An example
We recently wanted to engage with some key opinion leaders (KOLs) from oncology to understand their thoughts about liquid biopsies for the early detection of cancer. We contacted 13 lung cancer thought leaders to ask if they had time to take part in some research. Within a few hours we were pleased that we’d booked research sessions with three respondees.
Whilst COVID-19 is consuming our thoughts, we’re still keen to see where the liquid biopsies landscape is headed. The quick responses from the lung cancer specialists showed us that – despite the pandemic – physicians are also still passionate to take part in the discussions involving future advances for their therapy areas.
Eager to engage
Interestingly, two of the three physicians/KOLs we spoke to said how nice it was to have an ‘ordinary’ research discussion again about their specialist therapy area. This is extraordinary given the circumstances in which these physicians are working: their resources – human and otherwise – are being impacted, even commandeered to help fight the pandemic. One told the harrowing tale of losing seven of his seven-hundred strong medical team to the virus. Still, he wanted to fight on, not just against the virus but against cancer.
Unable to engage
Unsurprisingly, some of the other physicians declined, stating that ordinarily they would like to take part, but they are currently being pulled away from their own therapy areas to help the fight against COVID. This is a situation we understand and respect.
Press ahead with research for future advances, but with compassion
Our conclusion, which we thought worth sharing, is that so long as the topic is relevant, clinical thought leaders want to engage in market research that carries their specific area of scientific endeavour forward. They can see a future after the current pandemic, and so can we.
However, the healthcare system is really pulling together now; there is a single-minded goal to contain the pandemic. We cannot know who will and can engage and who cannot. It is for HCPs to decide if they can spare the time to get involved. Our approach: reach out cautiously, give them time to respond, work to their timetables, and if they don’t reply, don’t chase.
We’re pleased to report that over the last quarter we’ve recruited some excellent new joiners for both our UK and US offices. They’ve settled in nicely and we’re very excited that they’ve joined our team. Find out about each of them below.
Michelle Healy – Senior Research Executive
Michelle joined The Planning Shop in January as a Senior Research Executive. She previously worked at Blueprint Partnership where she gained experience in both qualitative and quantitative research.
Michelle studied at Newcastle University and enjoys playing Gaelic football and rugby in her spare time.
Michelle is based in our UK office.
Matt Barrett – Senior Research Executive
Matt has joined The Planning Shop as a Senior Research Executive direct from Naxion where he was a Senior Research Analyst. He has experience conducting both qualitative and quantitative research in healthcare and financial services.
Matt has a Bachelor’s Degree in Neuroscience from Lafayette College.
In his spare time, Matt enjoys playing and watching golf, cooking and trying new restaurants in Philadelphia. He also likes to visit the beach with friends, ski and snowboard, and watch Jeopardy!
Matt is from Philadelphia and is based in our US office.
Alyssa Turizo – Senior Research Executive
Alyssa joined The Planning Shop in February as a Senior Research Executive. She previously worked at Kudzu Research and Insights as a project manager, where she gained lots of experience conducting qualitative research projects.
Alyssa has a Bachelor and Master of Arts in Anthropology from the University of Pennsylvania. She is an avid potter, film enthusiast, bookworm and an urban hiker. Alyssa is based in our US office.
Trey Griffin – Research Manager
Trey joined The Planning Shop from Branding Science where he spent two years as a Research Executive working in both Quantitative and Qualitative research.
Trey has a Bachelor of Arts in History and International Relations, and a Master of Arts in Political Science and Government, both from the University of West Florida.
He is based in New Jersey, and he has an avid interest in international politics and board games. Trey also has a personal motto: “I not only use all the brains that I have, but all I can borrow.”
Trey is based in our US office.
Alicia Laing – Research Executive
Alicia joined The Planning Shop in February as a Research Executive.
She holds a degree in Biology from Swansea University and has spent the last couple of years working and travelling in Australia and Asia.
Alicia previously worked as a Research Associate at a market research agency called LRWTonic Ltd. Whilst she was there, she gained experience interviewing respondents, analysing results and working on both Qualitative and Quantitative projects.
In her spare time Alicia likes to travel, playing sport (lacrosse, skiing and hiking), enjoys music festivals and socialising with friends at the pub.
Alicia is based in our UK office.
Lucy Hannon – Research Executive
Lucy joined The Planning Shop as a research executive in mid-February.
As a recent graduate in Biological Sciences, Lucy wished to pursue a career in healthcare market research.
Lucy has a degree from The Royal Veterinary College. During her third-year dissertation she studied the effects of nutraceuticals on the cardiovascular system. She also spent part of her third year at Kings College London studying cardiovascular pharmacology and drug safety and toxicology.
Lucy has a strong passion for health and fitness. She enjoys playing Lacrosse, is an avid weightlifter and competes in bodybuilding competitions! She also enjoys baking and spending time with friends.
Lucy is based in our UK office.
Tessa Rothwell – Research Executive
Tessa is an ex-Science teacher who decided to move to a career in healthcare market research.
After working for Ipsos Mori (Healthcare) and Kantar Research where she was exposed to both qualitative and quantitative research, Tessa applied for a Research Executive role at The Planning Shop.
Tessa studied at the University of York and joined us in mid-February. She brings the following skills: project management, TabSpec writing, presentation designs, and liaising with support functions to ensure delivery to brief and within timelines.
Tessa is from Hanover, Germany, and enjoys spending time with her family, reading, rowing, playing the piano and photography.
Tessa is based in our UK office.
Atina Rashid – Business Support Executive
Atina joined the Resourcing Team as Business Support Executive in March. Her focus will be budgeting.
Atina comes from a data analytics background and has previously worked with Epsilon Abacus (a marketing and data analytic agency in Teddington). Whilst she was there she was responsible for collating, organising, processing and qualifying data for marketing activities.
In her spare time Atina likes to join her friends for dinner, watch movies and cooking. She also enjoys traveling and painting.
Atina is based in our UK office.
Stephen Pupkin – Senior Research Executive
Stephen freelanced with The Planning Shop for a few months before deciding to join us on a full-time basis.
He has extensive experience in healthcare market research having previously worked for BluePrint Research Group, Valeocon Management Consulting and Technical Resources International.
Stephen has a Bachelor’s degree in Neuroscience from John Hopkins University. He also has a Master’s in Biochemistry and Molecular Biology from Georgetown University.
Stephen is based in the New York area and will work from our US office.
Olivia Richmond – Global Quality System and Compliance Specialist
Olivia joined The Planning Shop in mid-March as a Global Quality System and Compliance Specialist. She will be working from our London office as will be a part of the Compliance Team.
This is a new type of role at The Planning Shop where Olivia will help to support the Adelphi Group Research Franchise (Adelphi and TPS) to align processes and procedures.
She will be supporting Adelphi Research (US/UK) in their ISO audit and helping TPS to achieve ISO certification. She will also provide support to help business units maintain and adhere to policies and SOPs, be compliant with all relevant country-specific legislation, including GDPR, all professional codes of conduct/practice, rules and regulations of regulatory agencies and client-specific policies and procedures; and provide some project compliance support.
Olivia has most recently worked as a Regulatory Submissions Coordinator for Medpace. She has a strong background in the pharma industry and applying GDPR/privacy regulations.
Olivia holds a BSc in Human Biology from the University of Loughborough.
In her spare time, Olivia enjoys travelling, baking (chocolate brownies being a firm favourite with her friends and family), taking on physical challenges (lacrosse and marathon running to mention a few), and seeing her friends and family.
Nick Diana – Senior Field Manager
Nick has joined The Planning Shop as a Senior Field Manager direct from Naxion where he was a Senior Operations Manager. He has significant experience conducting both qualitative and quantitative research in the healthcare space.
Nick has a Bachelor’s Degree in Finance from Pennsylvania State University.
Nick is the father of two daughters Selah (1 ½) and Chloe (3 weeks). In his limited free time, he enjoys playing and watching sports and playing strategy board games. He is also heavily involved in his local church. Nick is from Doylestown and is based in our US office.
Darja Idram – Research Director
Darja joined The Planning Shop from Elma Research. Her experience includes leading large leading large multidisciplinary teams in pharmaceutical, healthcare and public health research for more than a decade.
Darja has worked with multiple private sector, academic, government, and third-sector clients, delivering top quality applicable research and tangible client solutions. She has experience in both qualitative and quantitative research.
Darja has a degree and PhD in Sociology from Cambridge University.
If you’re interested in a career at The Planning Shop, please visit our Careers page.
The coronavirus pandemic is here, and 24-7 news coverage reports on the huge impact it’s having on health care providers. As market researchers we wanted to speak to physicians directly to understand the personal impact it is having on them. We also wanted to understand their views about the implications the pandemic will have on patient care, clinical trials and healthcare market research during this unprecedented time. We spoke to physicians in the US and UK working in areas that have had some of the highest numbers of COVID-19 to-date. Because of our place in healthcare, we’ve found it useful to understand physician’s thoughts, feelings and concerns, and we’ve highlighted some of these below. We hope you find these insights useful too.
How is the coronavirus pandemic impacting physicians’ day-to-day roles?
The level of impact varies greatly by specialty and in the US by practice setting (i.e. office vs. hospital), but all physicians have been impacted in some shape or form. At one end of the spectrum, we spoke with an endocrinologist in the US who closed her private practice and is now fielding patient phone calls (without reimbursement since the practice is not set up for telehealth), to a HEM-ONC who is still seeing patients but with a skeleton crew (meaning only her). In the UK, we heard from an oncologist who is shutting down two out of three oncology wards and is moving to a mixed ward consisting of oncology, care of the elderly, diabetes and endocrinology. The oncologist also told us that some of his oncology colleagues will be moving across to NHS Nightingale at London’s Excel Centre, to support the temporary hospital set up for COVID-19 cases. Physicians in both markets are doing what they can to minimise their oncology patients’ potential exposure to the virus as well as their own exposure, to preserve their health for a potentially all-hands-on-deck approach as the surge in COVID-19 cases approaches. In the US, some practices have laid off their administrative support staff, which has caused a lot of sadness and stress for providers.
Physicians who are in the midst of COVID-19 surges noted a few key changes:
(1) Days are longer than usual to cover for an influx in patients, and to cover for colleagues who have become sick;
(2) In the US, hospital-based PCPs are now working more hours within the Emergency Room as hospitalists, pulmonologists and infectious disease specialists have shifted to primarily testing and identifying COVID-19 cases.
(3) In the UK, PCPs are turning away all non-essential patients from the GP practice and fear a significant backlog of patients and buildup of undiagnosed conditions.
(4) Finally, across both markets some physicians are experiencing a new fear that they haven’t felt before: getting the disease they are treating patients for themselves, spreading the virus onto loved ones or seeing colleagues become sick.
Some specific comments from physicians:
“Preparing to care for very ill COVID-19 patients, it’s a bit of a draft. My transplant patients can be very ill, but I can’t bring their illness home to my family.”
– Academic Hem-Onc, Philadelphia, US
“We have stopped all procedures and only see patients with heart attacks or at risk of cardiac death. Therefore, half of the patients I’ve see today are COVID-19 patients. It isn’t my field but I’m trying to learn from my colleagues how to diagnose and treat these patients.”
– Cardiologist, Sheffield, UK
What does this mean for patient care and clinical trials?
Patient well-being is still the focus of HCPs, however they are having to change their approach to care. Oncology practices are still seeing patients who are undergoing active treatment (chemo suites are still up and running), but routine monitoring such as blood counts and regular follow up appointments have been paused or converted to telehealth. In the UK, oncology is taking this a little further where oncologists are making very hard decisions and will only treat patients where there is curative intent; the vast majority are otherwise having treatment delayed or even stopped. Physicians hope this will only be for 4-6 weeks but in oncology this is a long time, and even then, they do not know if there will be a ‘return-to-normal’ after 4-6 weeks. Doctors feel this is going to have a knock-on effect of a huge backlog of surgeries and treatments and it will impact the presentation and diagnosis of new cancers – essentially the whole pathway is being upturned. One hematology-oncologist in the US told us about a patient of hers who developed frozen shoulder and needed a steroid injection but can’t get it at this time so must manage the pain. Surgeons are paring down their practices, postponing elective procedures to limit exposure as well as to free up space with some operating theaters being turned into wards for COVID-19 patients. In a similar vein, ONCs are weighing the risk of potential coronavirus exposure with delayed monitoring. What the long-term effects of this will be is very much unknown, also the effect on patient volume, once it is safe to resume to ‘normal life’. Some ONCs are already halting clinical trial participation, others are continuing to participate but only for patients already enrolled or where there is no other possible treatment for the patient.
Some specific comments from physicians:
“I’m telling a lot of my patients to stay home…it’s not worth the risk.”
– Academic Hem-ONC, Philadelphia, US
“Science should move in parallel, not sequentially.”
– Cardiologist, New York, US
“You can only change the normal structure for so long: we will have a backlog of issues which will need to be dealt with eventually.”
– GP, London, UK
“Yesterday I talked to a patient who had disease progression and he’s interested in being treated, I’ve known him for a while…I have to judge over the phone whether he’s a candidate for treatment or not. Then his wife called and asked if he was going to die…these are conversations I would have liked to have in person, not over the phone.”
– Oncologist, Philadelphia, US
Is it ethical to continue market research during this time?
Doctors said yes, but that it’s important to be transparent about the topic as some HCPs may not be interested in less personally relevant topics. (HCPs were very interested in taking part in this interview though, given the topic was coronavirus). HCPs agree that normal life needs to continue, as does new drug development, and they feel market research provides them with an opportunity to contribute to this cause. Some HCPs — private practice or office-based practitioners in the US especially – have more time on their hands now that they are not seeing patients, and view market research as a welcome distraction. Some also view it as an important source of education and income, which is especially valuable during challenging times. They said that recruitment will need to be flexible based on practice setting (i.e. academics or those based in hospital settings may have less availability), specialty, and geography (for example, cities nearing their peaks – NYC, London – are to be avoided for a time).
Some specific comments from physicians:
“Physicians are happy to do these interviews because it gives extra income – most are bound to home.”
– Endo, Maryland, US
“I personally don’t think [conducting market research now] is an insensitive approach.”
– Cardiologist, New York, US
“The world moves on and this won’t reduce my appetite for market research. Generally we enjoy finding out about new treatments and new ideas.”
– Oncologist, London, UK
“Doctors are humans and we can’t work 24/7; we have homes and families and we like to do market research in our downtime, so it should still continue.”
– Cardiologist, London, UK
Sample: Research conducted by THE PLANNING SHOP 26 – 30 March 2020 with n=10 HCPs across the US and UK. US physicians were recruited from NYC, Philadelphia, DC areas. UK physicians recruited from London and the North. N=4 Oncologists, n=2 PCPs/GPs, n=2 Endocrinologists, n=2 Cardiologists.
Dear Friends, Colleagues and Partners,
With the advent and spread of the coronavirus we’ve entered unprecedented times. Times that we’ll no doubt look back upon in years to come and remember vividly because we’re all having to adapt at a rapid pace – day-by-day and hour-by-hour.
Speaking of adapting… as we navigate these unchartered waters, it’s not business as usual for us, but it is still delivery as usual. However, because the health and safety of our team members, clients, parents and families is our primary concern, we have made some changes to the way we work:We are all working from home instead of our offices.
We have eliminated all business travel.
We have increased access to a wealth of communication and file-sharing tools. This ensures we can all keep in touch with each other – and with you – whether it’s about a specific project, or simply to stay connected.
As we’re totally committed to assisting you with insight-led brand communications, we have also made some changes to the way we gather knowledge, for example, we’ve been re-engineering all our insight-gathering methodologies to ensure they are effective when conducted remotely.
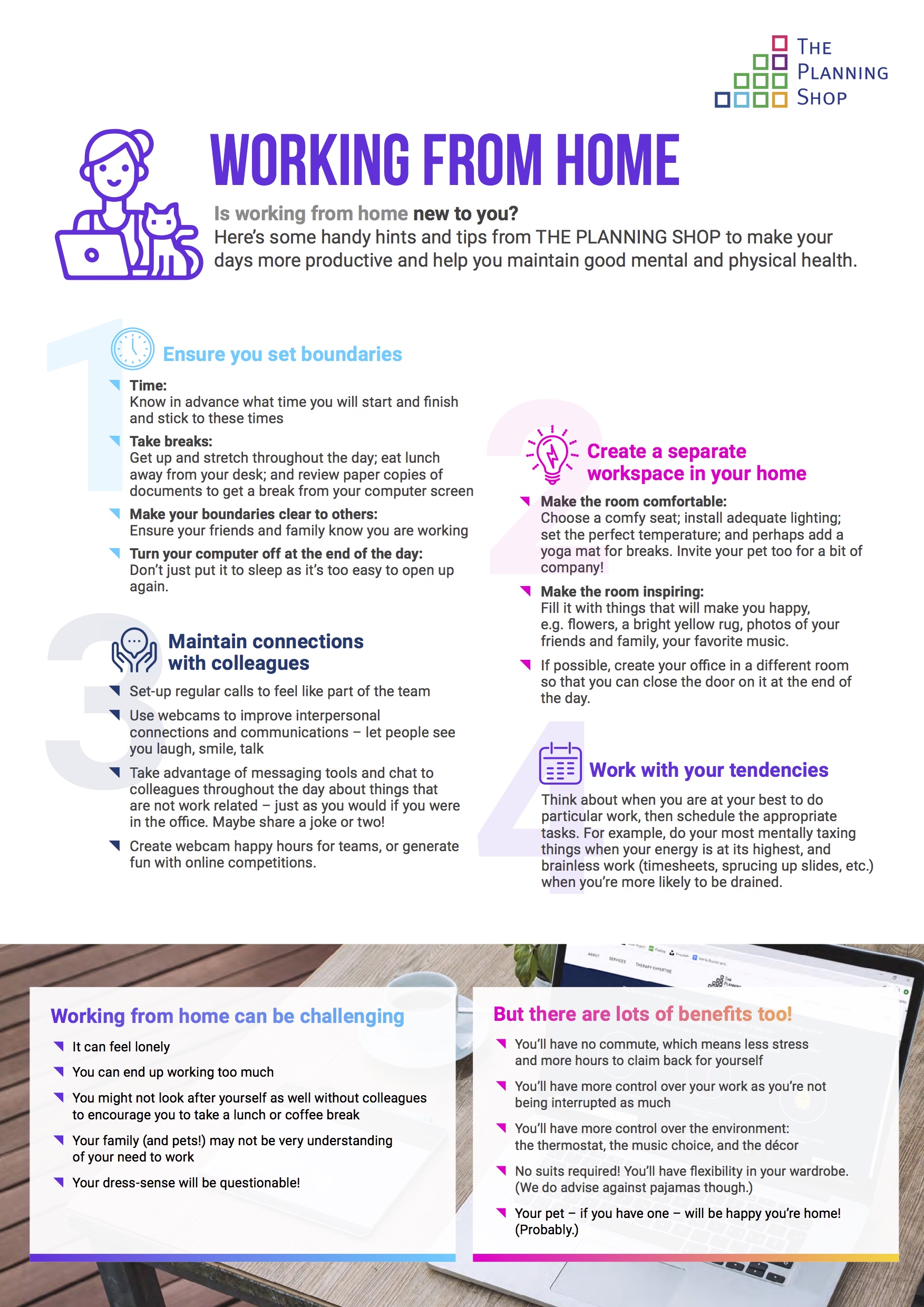
Sharing is caring! Work from home hints and tips
Working from home is becoming the new norm and the change in environment may be a struggle for some. If this is the case for you, we thought you might like to read our handy ‘Working from Home Hints and Tips Guide’. Because of the nature of our work, many of us have been working remotely for years and we think we have some pretty good advice to share!
Isolation shouldn’t be… isolating
Finally, for good mental health and to stay connected with fellow human beings, follow our social media channels where we’ll be posting all kinds of ‘light-relief’ news and information from our team members about their WFH adventures, favorite books, TV shows, cute pets, etc.
We’re on:
Instagram: @theplanningshop
Facebook: @theplanningshopintl
Twitter: @theplanningshop
Linkedin: @the-planning-shop-international
Feel free to get in touch too if you simply want someone new to talk to on any given day!
We hope you, your families and loved ones all stay safe and healthy over the coming months.
Take care,
From everyone at The Planning Shop
By Simon Barnes
May 2019 saw the BHBIA 2019 Annual Conference take place in the sunny, regal surroundings of Windsor. Not only was it the first time in recent years that the event was held outside the centre of London, but it was also the first year the BHBIA themed the conference with a variety of subjects instead of one over-arching topic. The diversity of subjects over the two days showcased so many amazing projects and bold ideas carried out by old and new faces across the industry, that team members and I from The Planning Shop were proud to be part of the event.

An emotional and inspirational keynote address from Anthony Bennett – a survivor of a devastating illness as a young adult – kick-started the conference. Anthony made the delegates think about how we order our priorities within the context of our everyday working lives and how we can ‘reboot’ our motivations to redefine our fears and recognise opportunity when it presents itself. His personal experiences, whilst clearly physically demanding, also highlighted the mental barriers we sometimes see without focussing on the strengths that come from clearing these hurdles.
Throughout the rest of the first day, several technology talks highlighted the opportunities that Artificial Intelligence (AI) is having on our industry now and in the future. Different perspectives were put forward about whether we should tread carefully in adopting these technologies or grasp them with both hands. Overall, delegates and speakers deemed that the reality of opportunity lies somewhere between AI complementing rather than replacing our industry’s traditional MR techniques.
In our home lives we are feeling our way and still exploring the opportunities that the Amazon Echo or Google Home (amongst others) present. With more and more companies entering the AI field, it is only a matter of time until this technology starts to make waves in our industry.

As always, the Gala BHBIA Evening Reception on day one gave everyone the opportunity to smarten up and celebrate the Best of Business Intelligence Awards (more affectionately known as the BOBIs) which continue to showcase outstanding performance across the UK Healthcare Market Research scene. As a representative from The Planning Shop I was delighted that our company was highly commended for the ‘Best Business Impact Award’ with our entry in partnership with Grünenthal. Whilst we didn’t win, we congratulate BMS and Strategic North for deservedly winning this highly competitive category – and we look forward to challenging them again next year!
I was also excited about the ‘Newcomer Category’ as our very own Rawaa Shami performed well in the final. I’ve been involved in judging this award for several years and in 2019 we saw some amazing entries and talent, none more so than Katharina Krasser from Ipsos who justifiably took home the trophy.
All award finalists and winners put an enormous amount of effort into their BOBI submissions across all categories (as well as completing the projects themselves) and they deserve every credit for their achievements – especially the winners!
The second day of the BHBIA conference moved into different areas with an interesting and thought-provoking paper hosted by Kantar Health offering a different perspective (to the discussion on day one by Anthony Bennett), about patients suffering from chronic illness. The talk focussed on how the devastation of a life-long chronic disease which is marginalised by society, creates isolation, depression and solitude which patients often hide from others. The mental anguish, as well as the associated physical pain of a chronic disease was demonstrated through the eyes of a patient – one who was extremely brave in sharing her experience at the BHBIA event. The session taught us that a condition trivialised in the media and wider society could be felt by the audience through a clever use of visual and auditory aids, as well as engaging techniques by the presenters who worked well to tell an effective, clear and impactful story.
The team behind the BHBIA 2019 Annual Conference did a great job in putting together a programme that covered a wide spectrum of themes, to an audience well represented by clients (research and analyst), agency, and fieldwork companies. As the BHBIA is, by definition, UK focussed it successfully managed to leverage our relatively close-knit community by taking a risk with its content, changing venue and location, and yet sticking to their reputation of presenting important and relevant information to key stakeholders across the industry. Long may this continue!
Well done BHBIA. Here’s to the 2020 conference!
About the author

Simon Barnes is Research Director at The Planning Shop with a focus on market research in the UK, covering all therapeutic areas. He has worked in pharmaceutical market research for over 20 years across several different therapeutic areas, including eye care in an international role. He leads the Ophthalmology Business Unit alongside his UK-specific role.
Download the pdf version here.